Obtaining fast and effective medical treatment after suffering and occupational accident or injury is important. Receiving the improper medication can made outcomes a lot worse The FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections and warns about disabling side effects that can occur together.
Copyright
(c) 2010-2024 Jon L Gelman, All Rights Reserved.
Showing posts sorted by date for query drugs. Sort by relevance Show all posts
Showing posts sorted by date for query drugs. Sort by relevance Show all posts
Monday, May 16, 2016
Wednesday, March 30, 2016
New safety warnings also added to all prescription opioid medications
 |
| FDA (Photo credit: Wikipedia) |
FDA announces enhanced warnings for immediate-release opioid pain medications related to risks of misuse, abuse, addiction, overdose and death. New safety warnings also added to all prescription opioid medications to inform prescribers and patients of additional risks related to opioid use.
Friday, March 18, 2016
NJ Judge Orders Psychotherapy Sessions In Conjunction With Pain Management
A NJ Workers' Compensation Judge Ordered the continuation of medical services to an injured worker who has been struggling for years because of chronic knee pain depression and anxiety despite the objection of the employer who sought to terminate care. The Judge Philip A. Tornetta, Administrative Supervisory Judge of Compensation, adopted an innovative approach in attempt to reduce or eliminated prescribed drugs including, "Oxycontin for her knee pain, Lexapro for depression and Xanax, which helps her sleep."
Wednesday, February 3, 2016
Workers’ Compensation and the Cancer Moonshot 2020
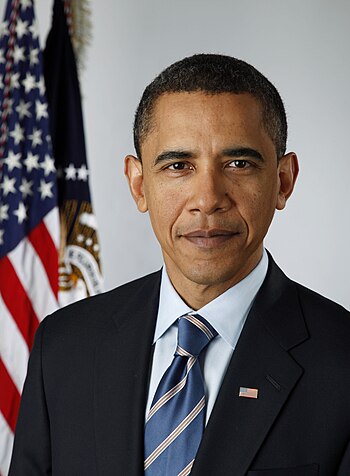
Official portrait of Vice President of the United States . (Photo credit: Wikipedia)
An exciting initiative, Cancer Moonshot 2020, is under underway establishing a coalition, of academics and insurers to work together to find a cure for cancer by the year 2020. Historically too many occupational exposures have resulted in the development of cancer. Participation by the entire workers’ compensation system in this new venture would create an exciting opportunity to advance worker health, reduce costs and strengthen the social remedial benefit program.
Wednesday, December 23, 2015
Should Workers' Compensation Be In The Wellness Business?
A recent study indicate that wellness programs are exceptionally important. Employers and workers' compensation insurance companies would be wise to follow this initiative.
One out of every four dollars employers pay for health care is tied to unhealthy lifestyle choices or conditions like smoking, stress and obesity, despite the fact that most large employers have workplace wellness programs.
One out of every four dollars employers pay for health care is tied to unhealthy lifestyle choices or conditions like smoking, stress and obesity, despite the fact that most large employers have workplace wellness programs.
Friday, December 18, 2015
CDC Reports Increases in Drug and Opioid Overdose Deaths in US 2000-2014
Workers' Compensation has experienced the consequences of the national epidemic of drug and opioid deaths. The issue continues to be reported and addressed at the national levels. Unfortunately employers and workers' compensation insurance companies, as cost cost containment item, continue to use this information to merely restrict drug benefits to injured workers while not meeting the real challenge of the epidemic.
The United States is experiencing an epidemic of drug overdose (poisoning) deaths. Since 2000, the rate of deaths from drug overdoses has increased 137%, including a 200% increase in the rate of overdose deaths involving opioids (opioid pain relievers and heroin). CDC analyzed recent multiple cause-of-death mortality data to examine current trends and characteristics of drug overdose deaths, including the types of opioids associated with drug overdose deaths. During 2014, a total of 47,055 drug overdose deaths occurred in the United States, representing a 1-year increase of 6.5%, from 13.8 per 100,000 persons in 2013 to 14.7 per 100,000 persons in 2014. The rate of drug overdose deaths increased significantly for both sexes, persons aged 25–44 years and ≥55 years, non-Hispanic whites and non-Hispanic blacks, and in the Northeastern, Midwestern, and Southern regions of the United States. Rates of opioid overdose deaths also increased significantly, from 7.9 per 100,000 in 2013 to 9.0 per 100,000 in 2014, a 14% increase. Historically, CDC has programmatically characterized all opioid pain reliever deaths (natural and semisynthetic opioids, methadone, and other synthetic opioids) as "prescription" opioid overdoses (1). Between 2013 and 2014, the age-adjusted rate of death involving methadone remained unchanged; however, the age-adjusted rate of death involving natural and semisynthetic opioid pain relievers, heroin, and synthetic opioids, other than methadone (e.g., fentanyl) increased 9%, 26%, and 80%, respectively. The sharp increase in deaths involving synthetic opioids, other than methadone, in 2014 coincided with law enforcement reports of increased availability of illicitly manufactured fentanyl, a synthetic opioid; however, illicitly manufactured fentanyl cannot be distinguished from prescription fentanyl in death certificate data. These findings indicate that the opioid overdose epidemic is worsening. There is a need for continued action to prevent opioid abuse, dependence, and death, improve treatment capacity for opioid use disorders, and reduce the supply of illicit opioids, particularly heroin and illicit fentanyl.
The National Vital Statistics System multiple cause-of-death mortality files were used to identify drug overdose deaths.* Drug overdose deaths were classified using the International Classification of Disease, Tenth Revision (ICD-10), based on the ICD-10 underlying cause-of-death codes X40–44 (unintentional), X60–64 (suicide), X85 (homicide), or Y10–Y14 (undetermined intent) (2). Among the deaths with drug overdose as the underlying cause, the type of opioid involved is indicated by the following ICD-10 multiple cause-of-death codes: opioids (T40.0, T40.1, T40.2, T40.3, T40.4, or T40.6); natural and semisynthetic opioids (T40.2); methadone (T40.3); synthetic opioids, other than methadone (T40.4); and heroin (T40.1). Some deaths involve more than one type of opioid; these deaths were included in the rates for each category (e.g., a death involving both a synthetic opioid and heroin would be included in the rates for synthetic opioid deaths and in the rates for heroin deaths). Age-adjusted death rates were calculated by applying age-specific death rates to the 2000 U.S standard population age distribution (3). Significance testing was based on the z-test at a significance level of 0.05.
During 2014, 47,055 drug overdose deaths occurred in the United States. Since 2000, the age-adjusted drug overdose death rate has more than doubled, from 6.2 per 100,000 persons in 2000 to 14.7 per 100,000 in 2014 (Figure 1). The overall number and rate of drug overdose deaths increased significantly from 2013 to 2014, with an additional 3,073 deaths occurring in 2014 (Table), resulting in a 6.5% increase in the age-adjusted rate. From 2013 to 2014, statistically significant increases in drug overdose death rates were seen for both males and females, persons aged 25–34 years, 35–44 years, 55–64 years, and ≥65 years; non-Hispanic whites and non-Hispanic blacks; and residents in the Northeast, Midwest and South Census Regions (Table). In 2014, the five states with the highest rates of drug overdose deaths were West Virginia (35.5 deaths per 100,000), New Mexico (27.3), New Hampshire (26.2), Kentucky (24.7) and Ohio(24.6).† States with statistically significant increases in the rate of drug overdose deaths from 2013 to 2014 included Alabama, Georgia, Illinois, Indiana, Maine, Maryland, Massachusetts, Michigan, New Hampshire, New Mexico, North Dakota, Ohio, Pennsylvania, and Virginia.
In 2014, 61% (28,647, data not shown) of drug overdose deaths involved some type of opioid, including heroin. The age-adjusted rate of drug overdose deaths involving opioids increased significantly from 2000 to 2014, increasing 14% from 2013 (7.9 per 100,000) to 2014 (9.0) (Figure 1). From 2013 to 2014, the largest increase in the rate of drug overdose deaths involved synthetic opioids, other than methadone (e.g., fentanyl and tramadol), which nearly doubled from 1.0 per 100,000 to 1.8 per 100,000 (Figure 2). Heroin overdose death rates increased by 26% from 2013 to 2014 and have more than tripled since 2010, from 1.0 per 100,000 in 2010 to 3.4 per 100,000 in 2014 (Figure 2). In 2014, the rate of drug overdose deaths involving natural and semisynthetic opioids (e.g., morphine, oxycodone, and hydrocodone), 3.8 per 100,000, was the highest among opioid overdose deaths, and increased 9% from 3.5 per 100,000 in 2013. The rate of drug overdose deaths involving methadone, a synthetic opioid classified separately from other synthetic opioids, was similar in 2013 and 2014.
Discussion
More persons died from drug overdoses in the United States in 2014 than during any previous year on record. From 2000 to 2014 nearly half a million persons in the United States have died from drug overdoses. In 2014, there were approximately one and a half times more drug overdose deaths in the United States than deaths from motor vehicle crashes (4). Opioids, primarily prescription pain relievers and heroin, are the main drugs associated with overdose deaths. In 2014, opioids were involved in 28,647 deaths, or 61% of all drug overdose deaths; the rate of opioid overdoses has tripled since 2000. The 2014 data demonstrate that the United States' opioid overdose epidemic includes two distinct but interrelated trends: a 15-year increase in overdose deaths involving prescription opioid pain relievers and a recent surge in illicit opioid overdose deaths, driven largely by heroin.
Natural and semisynthetic opioids, which include the most commonly prescribed opioid pain relievers, oxycodone and hydrocodone, continue to be involved in more overdose deaths than any other opioid type. Although this category of opioid drug overdose death had declined in 2012 compared with 2011, and had held steady in 2013, there was a 9% increase in 2014.
Drug overdose deaths involving heroin continued to climb sharply, with heroin overdoses more than tripling in 4 years. This increase mirrors large increases in heroin use across the country (5) and has been shown to be closely tied to opioid pain reliever misuse and dependence. Past misuse of prescription opioids is the strongest risk factor for heroin initiation and use, specifically among persons who report past-year dependence or abuse (5). The increased availability of heroin, combined with its relatively low price (compared with diverted prescription opioids) and high purity appear to be major drivers of the upward trend in heroin use and overdose (6).
The rate of drug overdose deaths involving synthetic opioids nearly doubled between 2013 and 2014. This category includes both prescription synthetic opioids (e.g., fentanyl and tramadol) and non-pharmaceutical fentanyl manufactured in illegal laboratories (illicit fentanyl). Toxicology tests used by coroners and medical examiners are unable to distinguish between prescription and illicit fentanyl. Based on reports from states and drug seizure data, however, a substantial portion of the increase in synthetic opioid deaths appears to be related to increased availability of illicit fentanyl (7), although this cannot be confirmed with mortality data. For example, five jurisdictions (Florida, Maryland, Maine, Ohio, and Philadelphia, Pennsylvania) that reported sharp increases in illicit fentanyl seizures, and screened persons who died from a suspected drug overdose for fentanyl, detected similarly sharp increases in fentanyl-relateddeaths (7).§ Finally, illicit fentanyl is often combined with heroin or sold as heroin. Illicit fentanyl might be contributing to recent increases in drug overdose deaths involving heroin. Therefore, increases in illicit fentanyl-associated deaths might represent an emerging and troubling feature of the rise in illicit opioid overdoses that has been driven by heroin.
The findings in this report are subject to at least three limitations. First, several factors related to death investigation might affect estimates of death rates involving specific drugs. At autopsy, toxicological laboratory tests might be performed to determine the type of drugs present; however, the substances tested for and circumstances under which the tests are performed vary by jurisdiction. Second, in 2013 and 2014, 22% and 19% of drug overdose deaths, respectively, did not include information on the death certificate about the specific types of drugs involved. The percent of overdose deaths with specific drugs identified on the death certificate varies widely by state. Some of these deaths might have involved opioids. This increase in the reporting of specific drugs in 2014 might have contributed to some of the observed increases in drug overdose death rates involving different types of opioids from 2013 to 2014. Finally, some heroin deaths might be misclassified as morphine because morphine and heroin are metabolized similarly (8), which might result in an underreporting of heroin overdose deaths.
To reverse the epidemic of opioid drug overdose deaths and prevent opioid-related morbidity, efforts to improve safer prescribing of prescription opioids must be intensified. Opioid pain reliever prescribing has quadrupled since 1999 and has increased in parallel with overdoses involving the most commonly used opioid pain relievers (1). CDC has developed a draft guideline for the prescribing of opioids for chronic pain to address this need.¶
In addition, efforts are needed to protect persons already dependent on opioids from overdose and other harms. This includes expanding access to and use of naloxone (a safe and effective antidote for all opioid-related overdoses)** and increasing access to medication-assisted treatment, in combination with behavioral therapies (9). Efforts to ensure access to integrated prevention services, including access to syringe service programs when available, is also an important consideration to prevent the spread of hepatitis C virus and human immunodeficiency virus infections from injection drug use.
Public health agencies, medical examiners and coroners, and law enforcement agencies can work collaboratively to improve detection of outbreaks of drug overdose deaths involving illicit opioids (including heroin and illicit fentanyl) through improved investigation and testing as well as reporting and monitoring of specific drugs, and facilitate a rapid and effective response that can address this emerging threat to public health and safety (7). Efforts are needed to distinguish the drugs contributing to overdoses to better understand this trend.
1Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, CDC.
Corresponding author: Rose A. Rudd, rvr2@cdc.gov, 770-488-3712.
The National Vital Statistics System multiple cause-of-death mortality files were used to identify drug overdose deaths.* Drug overdose deaths were classified using the International Classification of Disease, Tenth Revision (ICD-10), based on the ICD-10 underlying cause-of-death codes X40–44 (unintentional), X60–64 (suicide), X85 (homicide), or Y10–Y14 (undetermined intent) (2). Among the deaths with drug overdose as the underlying cause, the type of opioid involved is indicated by the following ICD-10 multiple cause-of-death codes: opioids (T40.0, T40.1, T40.2, T40.3, T40.4, or T40.6); natural and semisynthetic opioids (T40.2); methadone (T40.3); synthetic opioids, other than methadone (T40.4); and heroin (T40.1). Some deaths involve more than one type of opioid; these deaths were included in the rates for each category (e.g., a death involving both a synthetic opioid and heroin would be included in the rates for synthetic opioid deaths and in the rates for heroin deaths). Age-adjusted death rates were calculated by applying age-specific death rates to the 2000 U.S standard population age distribution (3). Significance testing was based on the z-test at a significance level of 0.05.
During 2014, 47,055 drug overdose deaths occurred in the United States. Since 2000, the age-adjusted drug overdose death rate has more than doubled, from 6.2 per 100,000 persons in 2000 to 14.7 per 100,000 in 2014 (Figure 1). The overall number and rate of drug overdose deaths increased significantly from 2013 to 2014, with an additional 3,073 deaths occurring in 2014 (Table), resulting in a 6.5% increase in the age-adjusted rate. From 2013 to 2014, statistically significant increases in drug overdose death rates were seen for both males and females, persons aged 25–34 years, 35–44 years, 55–64 years, and ≥65 years; non-Hispanic whites and non-Hispanic blacks; and residents in the Northeast, Midwest and South Census Regions (Table). In 2014, the five states with the highest rates of drug overdose deaths were West Virginia (35.5 deaths per 100,000), New Mexico (27.3), New Hampshire (26.2), Kentucky (24.7) and Ohio(24.6).† States with statistically significant increases in the rate of drug overdose deaths from 2013 to 2014 included Alabama, Georgia, Illinois, Indiana, Maine, Maryland, Massachusetts, Michigan, New Hampshire, New Mexico, North Dakota, Ohio, Pennsylvania, and Virginia.
In 2014, 61% (28,647, data not shown) of drug overdose deaths involved some type of opioid, including heroin. The age-adjusted rate of drug overdose deaths involving opioids increased significantly from 2000 to 2014, increasing 14% from 2013 (7.9 per 100,000) to 2014 (9.0) (Figure 1). From 2013 to 2014, the largest increase in the rate of drug overdose deaths involved synthetic opioids, other than methadone (e.g., fentanyl and tramadol), which nearly doubled from 1.0 per 100,000 to 1.8 per 100,000 (Figure 2). Heroin overdose death rates increased by 26% from 2013 to 2014 and have more than tripled since 2010, from 1.0 per 100,000 in 2010 to 3.4 per 100,000 in 2014 (Figure 2). In 2014, the rate of drug overdose deaths involving natural and semisynthetic opioids (e.g., morphine, oxycodone, and hydrocodone), 3.8 per 100,000, was the highest among opioid overdose deaths, and increased 9% from 3.5 per 100,000 in 2013. The rate of drug overdose deaths involving methadone, a synthetic opioid classified separately from other synthetic opioids, was similar in 2013 and 2014.
Discussion
More persons died from drug overdoses in the United States in 2014 than during any previous year on record. From 2000 to 2014 nearly half a million persons in the United States have died from drug overdoses. In 2014, there were approximately one and a half times more drug overdose deaths in the United States than deaths from motor vehicle crashes (4). Opioids, primarily prescription pain relievers and heroin, are the main drugs associated with overdose deaths. In 2014, opioids were involved in 28,647 deaths, or 61% of all drug overdose deaths; the rate of opioid overdoses has tripled since 2000. The 2014 data demonstrate that the United States' opioid overdose epidemic includes two distinct but interrelated trends: a 15-year increase in overdose deaths involving prescription opioid pain relievers and a recent surge in illicit opioid overdose deaths, driven largely by heroin.
Natural and semisynthetic opioids, which include the most commonly prescribed opioid pain relievers, oxycodone and hydrocodone, continue to be involved in more overdose deaths than any other opioid type. Although this category of opioid drug overdose death had declined in 2012 compared with 2011, and had held steady in 2013, there was a 9% increase in 2014.
Drug overdose deaths involving heroin continued to climb sharply, with heroin overdoses more than tripling in 4 years. This increase mirrors large increases in heroin use across the country (5) and has been shown to be closely tied to opioid pain reliever misuse and dependence. Past misuse of prescription opioids is the strongest risk factor for heroin initiation and use, specifically among persons who report past-year dependence or abuse (5). The increased availability of heroin, combined with its relatively low price (compared with diverted prescription opioids) and high purity appear to be major drivers of the upward trend in heroin use and overdose (6).
The rate of drug overdose deaths involving synthetic opioids nearly doubled between 2013 and 2014. This category includes both prescription synthetic opioids (e.g., fentanyl and tramadol) and non-pharmaceutical fentanyl manufactured in illegal laboratories (illicit fentanyl). Toxicology tests used by coroners and medical examiners are unable to distinguish between prescription and illicit fentanyl. Based on reports from states and drug seizure data, however, a substantial portion of the increase in synthetic opioid deaths appears to be related to increased availability of illicit fentanyl (7), although this cannot be confirmed with mortality data. For example, five jurisdictions (Florida, Maryland, Maine, Ohio, and Philadelphia, Pennsylvania) that reported sharp increases in illicit fentanyl seizures, and screened persons who died from a suspected drug overdose for fentanyl, detected similarly sharp increases in fentanyl-relateddeaths (7).§ Finally, illicit fentanyl is often combined with heroin or sold as heroin. Illicit fentanyl might be contributing to recent increases in drug overdose deaths involving heroin. Therefore, increases in illicit fentanyl-associated deaths might represent an emerging and troubling feature of the rise in illicit opioid overdoses that has been driven by heroin.
The findings in this report are subject to at least three limitations. First, several factors related to death investigation might affect estimates of death rates involving specific drugs. At autopsy, toxicological laboratory tests might be performed to determine the type of drugs present; however, the substances tested for and circumstances under which the tests are performed vary by jurisdiction. Second, in 2013 and 2014, 22% and 19% of drug overdose deaths, respectively, did not include information on the death certificate about the specific types of drugs involved. The percent of overdose deaths with specific drugs identified on the death certificate varies widely by state. Some of these deaths might have involved opioids. This increase in the reporting of specific drugs in 2014 might have contributed to some of the observed increases in drug overdose death rates involving different types of opioids from 2013 to 2014. Finally, some heroin deaths might be misclassified as morphine because morphine and heroin are metabolized similarly (8), which might result in an underreporting of heroin overdose deaths.
To reverse the epidemic of opioid drug overdose deaths and prevent opioid-related morbidity, efforts to improve safer prescribing of prescription opioids must be intensified. Opioid pain reliever prescribing has quadrupled since 1999 and has increased in parallel with overdoses involving the most commonly used opioid pain relievers (1). CDC has developed a draft guideline for the prescribing of opioids for chronic pain to address this need.¶
In addition, efforts are needed to protect persons already dependent on opioids from overdose and other harms. This includes expanding access to and use of naloxone (a safe and effective antidote for all opioid-related overdoses)** and increasing access to medication-assisted treatment, in combination with behavioral therapies (9). Efforts to ensure access to integrated prevention services, including access to syringe service programs when available, is also an important consideration to prevent the spread of hepatitis C virus and human immunodeficiency virus infections from injection drug use.
Public health agencies, medical examiners and coroners, and law enforcement agencies can work collaboratively to improve detection of outbreaks of drug overdose deaths involving illicit opioids (including heroin and illicit fentanyl) through improved investigation and testing as well as reporting and monitoring of specific drugs, and facilitate a rapid and effective response that can address this emerging threat to public health and safety (7). Efforts are needed to distinguish the drugs contributing to overdoses to better understand this trend.
1Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, CDC.
Corresponding author: Rose A. Rudd, rvr2@cdc.gov, 770-488-3712.
References
- Paulozzi LJ, Jones C, Mack K, Rudd R. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep 2011;60:1487–92.
- Bergen G, Chen LH, Warner M, Fingerhut LA. Injury in the United States: 2007 chartbook. Hyattsville, MD: National Center for Health Statistics; 2008 Available at http://www.cdc.gov/nchs/data/misc/injury2007.pdf
.
- Murphy SL, Xu JQ, Kochanek KD. Deaths: final data for 2010. National vital statistics reports. Hyattsville, MD: National Center for Health Statistics; 2013. Available at http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_04.pdf
.
- CDC. Wide-ranging online data for epidemiologic research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics; 2015. Available athttp://wonder.cdc.gov.
- Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users—United States, 2002–2013. MMWR Morb Mortal Wkly Rep 2015;64:719–25.
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past fifty years. JAMA Psychiatry 2014;71:821–6.
- CDC. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. HAN Health Advisory. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. Available at http://emergency.cdc.gov/han/han00384.asp.
- Davis GG. Complete republication: National Association of Medical Examiners position paper: recommendations for the investigation, diagnosis, and certification of deaths related to opioid drugs. J Med Toxicol 2014;10:100–6.
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med 2014;370:2063–6.
* Additional information available at http://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm.
† Additional information available at http://www.cdc.gov/drugoverdose/data/statedeaths.html.
§ Additional information available at http://pub.lucidpress.com/NDEWSFentanyl/ .
.
¶ Additional information available at http://www.cdc.gov/drugoverdose/prescribing/guideline.html.
** Additional information available at https://store.samhsa.gov/shin/content/SMA13-4742/Overdose_Toolkit_2014_Jan.pdf 
 .
.
Friday, July 10, 2015
FDA Strengthens NSAIDs Warnings: Chance of Heart Attack & Stroke
The U.S. Food and Drug Administration (FDA) is strengthening an existing label warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) increase the chance of a heart attack or stroke.
Based on the FDA's comprehensive review of new safety information, it is requiring updates to the drug labels of all prescription NSAIDs. As is the case with current prescription NSAID labels, the Drug Facts labels of over-the-counter (OTC) non-aspirin NSAIDs already contain information on heart attack and stroke risk. The FDA will also request updates to the OTC non-aspirin NSAID Drug Facts labels.
Patients taking NSAIDs should seek medical attention immediately if they experience symptoms such as chest pain, shortness of breath or trouble breathing, weakness in one part or side of their body, or slurred speech.
NSAIDs are widely used to treat pain and fever from many different long- and short-term medical conditions such as arthritis, menstrual cramps, headaches, colds, and the flu. NSAIDs are available by prescription and OTC. Examples of NSAIDs include ibuprofen, naproxen, diclofenac, and celecoxib (see Table 1 for a list of NSAIDs).
The risk of heart attack and stroke with NSAIDs, either of which can lead to death, was first described in 2005 in the Boxed Warning and Warnings and Precautions sections of the prescription drug labels. Since then, we have reviewed a variety of new safety information on prescription and OTC NSAIDs, including observational studies,1 a large combined analysis of clinical trials,2 and other scientific publications.1 These studies were also discussed at a joint meeting of the Arthritis Advisory Committee and Drug Safety and Risk Management Advisory Committee held on February 10-11, 2014.
Based on the FDA's review and the advisory committees’ recommendations, the prescription NSAID labels will be revised to reflect the following information:
It was previously thought that all NSAIDs may have a similar risk. Newer information makes it less clear that the risk for heart attack or stroke is similar for all NSAIDs; however, this newer information is not sufficient for us to determine that the risk of any particular NSAID is definitely higher or lower than that of any other particular NSAID.
NSAIDs can increase the risk of heart attack or stroke in patients with or without heart disease or risk factors for heart disease. A large number of studies support this finding, with varying estimates of how much the risk is increased, depending on the drugs and the doses studied.
In general, patients with heart disease or risk factors for it have a greater likelihood of heart attack or stroke following NSAID use than patients without these risk factors because they have a higher risk at baseline.
Patients treated with NSAIDs following a first heart attack were more likely to die in the first year after the heart attack compared to patients who were not treated with NSAIDs after their first heart attack.
There is an increased risk of heart failure with NSAID use.
In addition, the format and language contained throughout the labels of prescription NSAIDs will be updated to reflect the newest information available about the NSAID class.
Patients and health care professionals should remain alert for heart-related side effects the
entire time that NSAIDs are being taken. The FDA urges you to report side effects involving
NSAIDs to the FDA MedWatch program, using the information in the “Contact FDA”
box at the bottom of the page.
Facts about non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs)
• NSAIDs are a class of medicines available by prescription and over-the-counter
(OTC). They are some of the most commonly used pain medicines.
• NSAIDs are used to treat pain and fever from medical conditions such as arthritis,
menstrual cramps, headaches, colds, and the flu.
• Examples of NSAIDs include ibuprofen, naproxen, diclofenac, and celecoxib.
See Table 1 for a list of non-aspirin NSAIDs.
Additional Information for Patients and Consumers
• Non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) increase the chance
of a heart attack or stroke, either of which can lead to death. There are a large
number of studies that support this finding, with varying estimates of how much
the risk is increased, depending on the drugs and the doses studied. These serious
side effects can occur as early as the first weeks of using an NSAID and the risk
may increase the longer you are taking an NSAID.
• The risk appears greater at higher doses; use the lowest effective amount for the
shortest possible time.
• Seek medical attention immediately if you experience symptoms such as:
• Chest pain
• Shortness of breath or trouble breathing
• Sudden weakness or numbness in one part or side of the body
• Sudden slurred speech
• Many medicines contain NSAIDs, including those used for colds, flu, and sleep,
so it is important to read the labels and avoid taking multiple medicines that
contain NSAIDs.
• Patients who take low-dose aspirin for protection against heart attack and stroke
should know that some NSAIDs, including those in over-the-counter (OTC)
products such as ibuprofen and naproxen, can interfere with that protective effect.
• Read the patient Medication Guide you receive with your NSAID prescription. It
explains the risks associated with the use of the medicine. You may access
Medication Guides by clicking on this link.
• Read the Drug Facts label before taking an OTC NSAID. Talk to your health care
professional or pharmacist if you have questions or concerns about NSAIDs or
which medicines contain them.
• Report side effects from NSAIDs to the FDA MedWatch program, using the
information in the "Contact FDA" box at the bottom of this page.
Additional Information for Health Care Professionals
• Non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased
risk of serious cardiovascular thrombotic events, including myocardial infarction
and stroke, either of which can be fatal. There are a large number of studies that
support this finding, with varying estimates of how much the risk is increased.
Estimates of increased risk range from 10 percent to 50 percent or more,
depending on the drugs and the doses studied. This risk may occur as early as the
first weeks of treatment and may increase with duration of use.
• Remain alert for the development of cardiovascular adverse events throughout the
patient’s entire treatment course, even in the absence of previous cardiovascular
symptoms.
• Inform patients to seek medical attention immediately if they experience
symptoms of heart attack or stroke such as chest pain, shortness of breath or
trouble breathing, sudden weakness or numbness in one part or side of the body,
or sudden slurred speech.
• Encourage patients to read the Medication Guide for prescription NSAIDs and the
Drug Facts label for over-the-counter (OTC) NSAIDs.
• Based on available data, it is unclear whether the risk for cardiovascular
thrombotic events is similar for all non-aspirin NSAIDs.
• The increase in cardiovascular thrombotic risk has been observed most
consistently at higher doses.
• The relative increase in serious cardiovascular thrombotic events over baseline
conferred by NSAID use appears to be similar in those with and without known
cardiovascular disease or risk factors for cardiovascular disease. However,
patients with known cardiovascular disease or risk factors had a higher absolute
incidence of serious cardiovascular thrombotic events due to their increased
baseline rate.
• To minimize the risk for an adverse cardiovascular event in patients treated with
an NSAID, prescribe the lowest effective dose for the shortest duration possible.
• Some NSAIDs, including those in OTC products such as ibuprofen and naproxen,
can interfere with the antiplatelet action of low dose aspirin used for
cardioprotection by blocking aspirin’s irreversible COX-1 inhibition.
• Report adverse events involving NSAIDs to the FDA MedWatch program, using
the information in the "Contact FDA" box at the bottom of this page.
Data Summary
FDA reviewed a meta-analysis of randomized clinical trials of cardiovascular and upper
gastrointestinal events with non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs),
conducted by the Coxib and traditional NSAID Trialists’ (CNT) Collaboration of the
Clinical Trial Service and Epidemiological Studies Units at Oxford University.2
We also reviewed observational studies and other scientific publications in the medical literature.1
The findings of these studies were discussed at a joint meeting of the Arthritis Advisory
Committee and Drug Safety and Risk Management Advisory Committee held on
February 10-11, 2014 (for complete safety reviews, background information, and minutes
of this meeting, click here).
Based on the FDA's comprehensive review and the recommendations from the advisory committees, we are requiring label changes to reflect the following conclusions:
• A large number of studies support the finding that NSAIDs cause an increased
risk of serious cardiovascular thrombotic events, with varying estimates of how
much the risk is increased. Estimates of increased relative risk range from 10
percent to 50 percent or more, depending on the drugs and the doses studied.
• Several observational studies found a significant cardiovascular risk within days
to weeks of NSAID initiation. Some data also showed a higher risk with longer
NSAID treatment.
• There are observational data indicating that the thrombotic cardiovascular risk
from NSAID use is dose-related. There is also some evidence of this doseresponse
effect from clinical trials of celecoxib.
• Some observational studies and the CNT meta-analysis suggested that naproxen
may have a lower risk for cardiovascular thrombotic events compared to the other
NSAIDs; however, the observational studies and the indirect comparisons used in
the meta-analysis to assess the risk of the nonselective NSAIDs have limitations
that affect their interpretability. The variability in patients’ risk factors,
comorbidities, concomitant medications and drug interactions, doses being used,
duration of treatment, etc., also need to be taken into consideration to make valid
comparisons. Importantly, these studies were not designed to demonstrate
superior safety of one NSAID compared to another.
• There is evidence of an increased cardiovascular risk from NSAID use by
apparently healthy patients. Data from the CNT meta-analysis, individual
randomized controlled trials, and observational studies showed that the relative
increase in cardiovascular thrombotic events over baseline conferred by NSAID
use appears to be similar in those with and without known cardiovascular disease
or risk factors for cardiovascular disease. However, patients with known
cardiovascular disease or risk factors had a higher absolute incidence of excess
cardiovascular thrombotic events due to their increased baseline rate.
• The CNT meta-analysis demonstrated an approximately two-fold increase in
hospitalizations for heart failure with use of both COX-2 selective and
nonselective NSAIDs. In a Danish National Registry study of patients with heart
failure, NSAID use increased the risk of myocardial infarction, hospitalization for
heart failure, and death.
The Prospective Randomized Evaluation of Celecoxib Integrated Safety versus Ibuprofen
or Naproxen (PRECISION) trial, is a large, ongoing randomized safety trial comparing
cardiovascular event rates among patients with high cardiovascular risk who are
randomized to celecoxib, naproxen, or ibuprofen. This trial was also discussed at the
February 2014 Advisory Committee meeting and is expected to provide additional safety
information.
Table 1. List of non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs)
Generic name Brand name(s)
References
1. Food and Drug Administration [Internet]. Silver Spring, MD. FDA Briefing
Information for the February 10-11, 2014 Joint Meeting of the Arthritis Advisory
Committee and Drug Safety and Risk Management Advisory Committee. Available
from:
http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM383180.pdf. Accessed December 23, 2014.
Based on the FDA's comprehensive review of new safety information, it is requiring updates to the drug labels of all prescription NSAIDs. As is the case with current prescription NSAID labels, the Drug Facts labels of over-the-counter (OTC) non-aspirin NSAIDs already contain information on heart attack and stroke risk. The FDA will also request updates to the OTC non-aspirin NSAID Drug Facts labels.
Patients taking NSAIDs should seek medical attention immediately if they experience symptoms such as chest pain, shortness of breath or trouble breathing, weakness in one part or side of their body, or slurred speech.
NSAIDs are widely used to treat pain and fever from many different long- and short-term medical conditions such as arthritis, menstrual cramps, headaches, colds, and the flu. NSAIDs are available by prescription and OTC. Examples of NSAIDs include ibuprofen, naproxen, diclofenac, and celecoxib (see Table 1 for a list of NSAIDs).
The risk of heart attack and stroke with NSAIDs, either of which can lead to death, was first described in 2005 in the Boxed Warning and Warnings and Precautions sections of the prescription drug labels. Since then, we have reviewed a variety of new safety information on prescription and OTC NSAIDs, including observational studies,1 a large combined analysis of clinical trials,2 and other scientific publications.1 These studies were also discussed at a joint meeting of the Arthritis Advisory Committee and Drug Safety and Risk Management Advisory Committee held on February 10-11, 2014.
Based on the FDA's review and the advisory committees’ recommendations, the prescription NSAID labels will be revised to reflect the following information:
- The risk of heart attack or stroke can occur as early as the first weeks of using an NSAID. The risk may increase with longer use of the NSAID.
- The risk appears greater at higher doses.
It was previously thought that all NSAIDs may have a similar risk. Newer information makes it less clear that the risk for heart attack or stroke is similar for all NSAIDs; however, this newer information is not sufficient for us to determine that the risk of any particular NSAID is definitely higher or lower than that of any other particular NSAID.
NSAIDs can increase the risk of heart attack or stroke in patients with or without heart disease or risk factors for heart disease. A large number of studies support this finding, with varying estimates of how much the risk is increased, depending on the drugs and the doses studied.
In general, patients with heart disease or risk factors for it have a greater likelihood of heart attack or stroke following NSAID use than patients without these risk factors because they have a higher risk at baseline.
Patients treated with NSAIDs following a first heart attack were more likely to die in the first year after the heart attack compared to patients who were not treated with NSAIDs after their first heart attack.
There is an increased risk of heart failure with NSAID use.
In addition, the format and language contained throughout the labels of prescription NSAIDs will be updated to reflect the newest information available about the NSAID class.
Patients and health care professionals should remain alert for heart-related side effects the
entire time that NSAIDs are being taken. The FDA urges you to report side effects involving
NSAIDs to the FDA MedWatch program, using the information in the “Contact FDA”
box at the bottom of the page.
Facts about non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs)
• NSAIDs are a class of medicines available by prescription and over-the-counter
(OTC). They are some of the most commonly used pain medicines.
• NSAIDs are used to treat pain and fever from medical conditions such as arthritis,
menstrual cramps, headaches, colds, and the flu.
• Examples of NSAIDs include ibuprofen, naproxen, diclofenac, and celecoxib.
See Table 1 for a list of non-aspirin NSAIDs.
Additional Information for Patients and Consumers
• Non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) increase the chance
of a heart attack or stroke, either of which can lead to death. There are a large
number of studies that support this finding, with varying estimates of how much
the risk is increased, depending on the drugs and the doses studied. These serious
side effects can occur as early as the first weeks of using an NSAID and the risk
may increase the longer you are taking an NSAID.
• The risk appears greater at higher doses; use the lowest effective amount for the
shortest possible time.
• Seek medical attention immediately if you experience symptoms such as:
• Chest pain
• Shortness of breath or trouble breathing
• Sudden weakness or numbness in one part or side of the body
• Sudden slurred speech
• Many medicines contain NSAIDs, including those used for colds, flu, and sleep,
so it is important to read the labels and avoid taking multiple medicines that
contain NSAIDs.
• Patients who take low-dose aspirin for protection against heart attack and stroke
should know that some NSAIDs, including those in over-the-counter (OTC)
products such as ibuprofen and naproxen, can interfere with that protective effect.
• Read the patient Medication Guide you receive with your NSAID prescription. It
explains the risks associated with the use of the medicine. You may access
Medication Guides by clicking on this link.
• Read the Drug Facts label before taking an OTC NSAID. Talk to your health care
professional or pharmacist if you have questions or concerns about NSAIDs or
which medicines contain them.
• Report side effects from NSAIDs to the FDA MedWatch program, using the
information in the "Contact FDA" box at the bottom of this page.
Additional Information for Health Care Professionals
• Non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased
risk of serious cardiovascular thrombotic events, including myocardial infarction
and stroke, either of which can be fatal. There are a large number of studies that
support this finding, with varying estimates of how much the risk is increased.
Estimates of increased risk range from 10 percent to 50 percent or more,
depending on the drugs and the doses studied. This risk may occur as early as the
first weeks of treatment and may increase with duration of use.
• Remain alert for the development of cardiovascular adverse events throughout the
patient’s entire treatment course, even in the absence of previous cardiovascular
symptoms.
• Inform patients to seek medical attention immediately if they experience
symptoms of heart attack or stroke such as chest pain, shortness of breath or
trouble breathing, sudden weakness or numbness in one part or side of the body,
or sudden slurred speech.
• Encourage patients to read the Medication Guide for prescription NSAIDs and the
Drug Facts label for over-the-counter (OTC) NSAIDs.
• Based on available data, it is unclear whether the risk for cardiovascular
thrombotic events is similar for all non-aspirin NSAIDs.
• The increase in cardiovascular thrombotic risk has been observed most
consistently at higher doses.
• The relative increase in serious cardiovascular thrombotic events over baseline
conferred by NSAID use appears to be similar in those with and without known
cardiovascular disease or risk factors for cardiovascular disease. However,
patients with known cardiovascular disease or risk factors had a higher absolute
incidence of serious cardiovascular thrombotic events due to their increased
baseline rate.
• To minimize the risk for an adverse cardiovascular event in patients treated with
an NSAID, prescribe the lowest effective dose for the shortest duration possible.
• Some NSAIDs, including those in OTC products such as ibuprofen and naproxen,
can interfere with the antiplatelet action of low dose aspirin used for
cardioprotection by blocking aspirin’s irreversible COX-1 inhibition.
• Report adverse events involving NSAIDs to the FDA MedWatch program, using
the information in the "Contact FDA" box at the bottom of this page.
Data Summary
FDA reviewed a meta-analysis of randomized clinical trials of cardiovascular and upper
gastrointestinal events with non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs),
conducted by the Coxib and traditional NSAID Trialists’ (CNT) Collaboration of the
Clinical Trial Service and Epidemiological Studies Units at Oxford University.2
We also reviewed observational studies and other scientific publications in the medical literature.1
The findings of these studies were discussed at a joint meeting of the Arthritis Advisory
Committee and Drug Safety and Risk Management Advisory Committee held on
February 10-11, 2014 (for complete safety reviews, background information, and minutes
of this meeting, click here).
Based on the FDA's comprehensive review and the recommendations from the advisory committees, we are requiring label changes to reflect the following conclusions:
• A large number of studies support the finding that NSAIDs cause an increased
risk of serious cardiovascular thrombotic events, with varying estimates of how
much the risk is increased. Estimates of increased relative risk range from 10
percent to 50 percent or more, depending on the drugs and the doses studied.
• Several observational studies found a significant cardiovascular risk within days
to weeks of NSAID initiation. Some data also showed a higher risk with longer
NSAID treatment.
• There are observational data indicating that the thrombotic cardiovascular risk
from NSAID use is dose-related. There is also some evidence of this doseresponse
effect from clinical trials of celecoxib.
• Some observational studies and the CNT meta-analysis suggested that naproxen
may have a lower risk for cardiovascular thrombotic events compared to the other
NSAIDs; however, the observational studies and the indirect comparisons used in
the meta-analysis to assess the risk of the nonselective NSAIDs have limitations
that affect their interpretability. The variability in patients’ risk factors,
comorbidities, concomitant medications and drug interactions, doses being used,
duration of treatment, etc., also need to be taken into consideration to make valid
comparisons. Importantly, these studies were not designed to demonstrate
superior safety of one NSAID compared to another.
• There is evidence of an increased cardiovascular risk from NSAID use by
apparently healthy patients. Data from the CNT meta-analysis, individual
randomized controlled trials, and observational studies showed that the relative
increase in cardiovascular thrombotic events over baseline conferred by NSAID
use appears to be similar in those with and without known cardiovascular disease
or risk factors for cardiovascular disease. However, patients with known
cardiovascular disease or risk factors had a higher absolute incidence of excess
cardiovascular thrombotic events due to their increased baseline rate.
• The CNT meta-analysis demonstrated an approximately two-fold increase in
hospitalizations for heart failure with use of both COX-2 selective and
nonselective NSAIDs. In a Danish National Registry study of patients with heart
failure, NSAID use increased the risk of myocardial infarction, hospitalization for
heart failure, and death.
The Prospective Randomized Evaluation of Celecoxib Integrated Safety versus Ibuprofen
or Naproxen (PRECISION) trial, is a large, ongoing randomized safety trial comparing
cardiovascular event rates among patients with high cardiovascular risk who are
randomized to celecoxib, naproxen, or ibuprofen. This trial was also discussed at the
February 2014 Advisory Committee meeting and is expected to provide additional safety
information.
Table 1. List of non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs)
Generic name Brand name(s)
- celecoxib Celebrex
- diclofenac Cambia, Cataflam, Dyloject, Flector,
- Pennsaid, Solaraze, Voltaren, Voltaren-XR,
- Zipsor, Zorvolex, Arthrotec (combination
- with misoprostol)
- diflunisal No brand name currently marketed
- etodolac No brand name currently marketed
- fenoprofen Nalfon
- flurbiprofen Ansaid
- ibuprofen* Advil, Caldolor, Children’s Advil,
- Children’s Elixsure IB, Children’s Motrin,
- Ibu-Tab, Ibuprohm, Motrin IB, Motrin
- Migraine Pain, Profen, Tab-Profen, Duexis
- (combination with famotidine), Reprexain
- (combination with hydrocodone),
- Vicoprofen (combination with
- hydrocodone)
- indomethacin Indocin, Tivorbex
- ketoprofen No brand name currently marketed
- ketorolac Sprix
- mefenamic acid Ponstel
- meloxicam Mobic
- nabumetone No brand name currently marketed
- naproxen* Aleve, Anaprox, Anaprox DS, ECNaprosyn,
- Naprelan, Naprosyn, Treximet
- (combination with sumatriptan), Vimovo
- (combination with esomeprazole)
- oxaprozin Daypro
- piroxicam Feldene
- sulindac Clinoril
- tolmetin No brand name currently marketed *There are many over-the-counter (OTC) products that contain this medicine.
References
1. Food and Drug Administration [Internet]. Silver Spring, MD. FDA Briefing
Information for the February 10-11, 2014 Joint Meeting of the Arthritis Advisory
Committee and Drug Safety and Risk Management Advisory Committee. Available
from:
http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM383180.pdf. Accessed December 23, 2014.
….
Jon L. Gelman of Wayne NJ is the author of NJ Workers’ Compensation Law (West-Thompson-Reuters) and co-author of the national treatise, Modern Workers’ Compensation Law (West-Thompson-Reuters). For over 4 decades the Law Offices of Jon L Gelman 1.973.696.7900 jon@gelmans.com have been representing injured workers and their families who have suffered occupational accidents and illnesses.
Related articles
- Pain Relievers Maybe Complicating Workers' Compensation Claims (workers-compensation.blogspot.com)
- FDA warns of rare but serious risk of heart attack and death with cardiac nuclear stress test drugs Lexiscan (regadenoson) and Adenoscan (adenosine) (workers-compensation.blogspot.com)
- Preventing Heart Attacks in Firefighters (workers-compensation.blogspot.com)
- Researchers Shed Light on Link Between Stress, Heart Trouble (workers-compensation.blogspot.com)
Tuesday, May 5, 2015
Look Who Is Prescribing What
As part of the Administration’s goals of better, care, smarter spending, and healthier people, the Centers for Medicare & Medicaid Services announced the availability of new, privacy-protected data on Medicare Part D prescription drugs prescribed by physicians and other health care professionals in 2013. This data shows which prescription drugs were prescribed to Medicare Part D beneficiaries by which practitioners.
CMS Defines Further Defines Policy Implementation on Part D Coverage of Benzodiazepines and Barbiturates (workers-compensation.blogspot.com)
Study: Cancer costs 'skyrocketed' despite drug cuts (workers-compensation.blogspot.com)
Big Pharma: More corruption reported in the architecture of evidence based medicine (workers-compensation.blogspot.com)
Public Comment Sought on Draft Document for Workplace Tobacco Policies (workers-compensation.blogspot.com)
“This transparency will give patients, researchers, and providers access to information that will help shape the future of our nation’s health for the better,” said acting CMS Administrator Andy Slavitt. “Beneficiaries’ personal information is not available; however, it’s important for consumers, their providers, researchers, and other stakeholders to know how many prescription drugs are prescribed and how much they cost the health care system, so that they can better understand how the Medicare Part D program delivers care.”
The new data set contains information from over one million distinct health care providers who collectively prescribed approximately $103 billion in prescription drugs and supplies paid under the Part D program. The data characterizes the individual prescribing patterns of health providers that participate in Medicare Part D for over 3,000 distinct drug products. For each prescriber and drug, the dataset includes the total number of prescriptions that were dispensed, which include original prescriptions and any refills, and the total drug cost paid by beneficiaries, Part D plans, and other sources.
CMS created the new data set using drug claim information submitted by Medicare Advantage Prescription Drug plans and stand-alone Prescription Drug Plans. With this data, it will be possible to conduct a wide array of prescription drug analyses that compare drug use and costs for specific providers, brand versus generic drug prescribing rates, and to make geographic comparisons at the state level.
The Administration has set measurable goals and a timeline to move Medicare toward paying providers based on the quality, rather than the quantity, of care they give patients. This is part of a wide set of initiatives to achieve better care, smarter spending and healthier people through our health care system. Open sharing of data securely, timely and more broadly supports insight and innovation in health care delivery.
Today’s Part D prescriber data availability adds to the unprecedented information previously released on services and procedures provided to Medicare beneficiaries, including hospital charge data on common impatient and outpatient services as well as utilization and payment information for physicians and other healthcare professionals. In addition, under the Qualified Entity (QE) program, CMS releases Medicare data to approved entities for the purposes of producing public performance reports on physicians, hospitals, and other providers. To date, CMS has certified 11 regional QEs and one national QE.
To view a fact sheet on the Medicare Part D prescriber data, visit: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Part-D-Prescriber.html
Updated: May 15, 2015
Related articles
How Proposed Part D Changes Are Playing On Capitol Hill (workers-compensation.blogspot.com)
The new data set contains information from over one million distinct health care providers who collectively prescribed approximately $103 billion in prescription drugs and supplies paid under the Part D program. The data characterizes the individual prescribing patterns of health providers that participate in Medicare Part D for over 3,000 distinct drug products. For each prescriber and drug, the dataset includes the total number of prescriptions that were dispensed, which include original prescriptions and any refills, and the total drug cost paid by beneficiaries, Part D plans, and other sources.
CMS created the new data set using drug claim information submitted by Medicare Advantage Prescription Drug plans and stand-alone Prescription Drug Plans. With this data, it will be possible to conduct a wide array of prescription drug analyses that compare drug use and costs for specific providers, brand versus generic drug prescribing rates, and to make geographic comparisons at the state level.
The Administration has set measurable goals and a timeline to move Medicare toward paying providers based on the quality, rather than the quantity, of care they give patients. This is part of a wide set of initiatives to achieve better care, smarter spending and healthier people through our health care system. Open sharing of data securely, timely and more broadly supports insight and innovation in health care delivery.
Today’s Part D prescriber data availability adds to the unprecedented information previously released on services and procedures provided to Medicare beneficiaries, including hospital charge data on common impatient and outpatient services as well as utilization and payment information for physicians and other healthcare professionals. In addition, under the Qualified Entity (QE) program, CMS releases Medicare data to approved entities for the purposes of producing public performance reports on physicians, hospitals, and other providers. To date, CMS has certified 11 regional QEs and one national QE.
To view a fact sheet on the Medicare Part D prescriber data, visit: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Part-D-Prescriber.html
Updated: May 15, 2015
Related articles
How Proposed Part D Changes Are Playing On Capitol Hill (workers-compensation.blogspot.com)
CMS Defines Further Defines Policy Implementation on Part D Coverage of Benzodiazepines and Barbiturates (workers-compensation.blogspot.com)
Study: Cancer costs 'skyrocketed' despite drug cuts (workers-compensation.blogspot.com)
Big Pharma: More corruption reported in the architecture of evidence based medicine (workers-compensation.blogspot.com)
Public Comment Sought on Draft Document for Workplace Tobacco Policies (workers-compensation.blogspot.com)
Sunday, May 3, 2015
Synchromed II Implantable Infusion Pump Systems: FDA Consent Decree To Limit Use
Medtronic, Inc. cited for manufacturing violations
The U.S. Food and Drug Administration announced today the filing of a consent decree against Medtronic, Inc., and two of the company’s officers—S. Omar Ishrak and Thomas M. Tefft —for repeatedly failing to correct violations, related to the manufacture of Synchromed II Implantable Infusion Pump Systems, medical devices that deliver medication to treat primary or metastatic cancer, chronic pain and severe spasticity. These violations occurred at the company’s Neuromodulation facilities in Columbia Heights, Minnesota, where the devices are manufacture.
The consent decree cites violations of the quality system regulation for medical devices, which requires manufacturers to have processes in place to assure that the design, manufacture and distribution of a device allows for its safe us
The legal action requires the company to stop manufacturing, designing and distributing new Synchromed II Implantable Infusion Pump Systems except in very limited cases, such as when a physician determines that the Synchromed II Implantable Infusion Pump System is medically necessary for a patient’s treatment.
The consent decree also requires Medtronic to retain a third-party expert to help develop and submit plans to the FDA to correct violations. The consent decree will remain in effect until the FDA has determined that Medtronic has met all the provisions listed in the consent decree.
Once Medtronic receives permission from the FDA to resume the design, manufacture and distribution of these products, the company must continue to submit audit reports so the agency can verify the company’s compliance. In addition to these audits, the FDA will monitor the company’s activities through its own inspections.
The FDA first approved the Synchromed II Implantable Infusion Pump Systems in 2004, and first identified problems with the manufacture of these pumps in 2006. These problems can result in over- or under-infusion or a delay in therapy for patients.
Between 2006 and 2013, FDA investigators conducted five inspections at Medtronic’s Neuromodulation facilities, resulting in three warning letters notifying the company of major violations. The violations included inadequate processes for identifying, investigating, and correcting quality problems with the Synchromed II Implantable Infusion Pump Systems; failure to document design changes; and failure to ensure that finished products meet design specifications.
“The FDA expects that all patients will be treated with safe, effective and high-quality medical devices,” said Jan Welch, acting director of the Office of Compliance in the FDA’s Center for Devices and Radiological Health. “We will continue to stop distribution of devices made by firms that fall short of regulatory requirements.”
Patients who are implanted with a Synchromed II Implantable Infusion Pump System should maintain regular follow-up appointments with their physicians. Patients who experience a change or return of symptoms, or hear a device alarm, should contact their physician immediately.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety and effectiveness of human and veterinary drugs, biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
Related articles
- FDA tells Nashville pharmacy to correct problems (workers-compensation.blogspot.com)
- FDA issues safety communication on HeartStart automated external defibrillators from Philips Healthcare (workers-compensation.blogspot.com)
- FDA approves device that helps people with certain spinal cord injuries to walk (workers-compensation.blogspot.com)
- Class I Recall: Medtronic's Worldwide Voluntary Field Action on Guidewires (workers-compensation.blogspot.com)
Thursday, February 5, 2015
Budget Changes To Medicare, HHS Programs Would Garner $399 Billion In 10 Years
The Obama Administration is making a concerted effort to lower medical costs through budgetary restrictions. It is unknown whether this is really meant to merely reduce service or establish greater efficiency. The CMS program is the model for the majority workers' compensation medical cost schedules. Today's post was shared by Kaiser Health News and comes from kaiserhealthnews.org
The New York Times: Budget Plan Sees Savings In Changes To Medicare In his new budget, President Obama proposed on Monday to squeeze $399 billion over the next 10 years out of Medicare, Medicaid and other programs run by the Department of Health and Human Services. Under the proposals, many Medicare beneficiaries would have to pay more for their care and coverage. The president would, for example, introduce a co-payment for new Medicare beneficiaries who receive home health care services, and he would collect $4 billion over 10 years by imposing a surcharge on premiums for new beneficiaries who buy generous private insurance to supplement Medicare. (Pear, 2/2) The Wall Street Journal: Obama Health Budget Calls For Authority To Negotiate Drug Prices The Obama administration’s fiscal 2016 budget request calls for allowing the government to negotiate the price of prescription drugs and giving regulators new funding to fight Ebola. The Department of Health and Human Services request proposes a budget authority of about $1.09 trillion for fiscal 2016, up from $1.04... |
….
Jon L. Gelman of Wayne NJ is the author of NJ Workers’ Compensation Law (West-Thompson-Reuters) and co-author of the national treatise, Modern Workers’ Compensation Law (West-Thompson-Reuters). For over 4 decades the Law Offices of Jon L Gelman 1.973.696.7900 jon@gelmans.com have been representing injured workers and their families who have suffered occupational accidents and illnesses.
Related articles
- Where We Are With Obamacare And Where We're Going (workers-compensation.blogspot.com)
- Why does health care cost so much in America? Ask Harvard's David Cutler (workers-compensation.blogspot.com)
- Obama Vows Better Health Care, Other Initiatives, For Vets, Military (workers-compensation.blogspot.com)
Saturday, January 24, 2015
A Video Interview Of Benjamin Marcus: The History of Workers' Compensation
Attorney Benjamin Marcus, the 1946 founding president of NACCA (The National Association of Compensation Claimants Attorneys), was interviewed by attorneys: N. Michael Rucka, Karen Spencer, Timothy Bott and Roy Portenga. The interview took place on January 1, 1997 in Michigan.
The video project was inspired by N. Michael Rucka under his leadership of WILG (Workplace Injury Litigation Group). WILG was originally created as a litigation group of ATLA (The Association of Trial Lawyers of America). Subsequently, WILG established itself as an independent organization.
NACCA eventual expanded by became ATLA (The Association of Trial Lawyers of America) and is now known as AAJ (The American Association for Justice).
Related articles
- House Considers Bills to Limit Americans' Rights (workers-compensation.blogspot.com)
- AAJ Responds To WSJ Report About Rising Asbestos Claims (workers-compensation.blogspot.com)
- Video: AAJ President Discusses Generic Drugs (workers-compensation.blogspot.com)
- Trucking Insurance Minimums Must be Raised to Make Our Roads Safer (workers-compensation.blogspot.com)
- The Affordable Care Act and Workers' Compensation: The Known Unknowns (workers-compensation.blogspot.com)
- U.S. Chamber's Hypocrisy Exposed: Do As I Say, Not As I Sue (workers-compensation.blogspot.com)
Sunday, January 11, 2015
High Compensation Medical Costs Raises Concern in New Hampshire
Medical costs now constitute a huge percentage of every workers' compensation claim. A recent editorial published in New Hampshire asserts that soaring and unequal medical costs have broken the workers' compensation system. Today's post is shared from concordmonitor.com/
Lawmakers should make 2014 the last year that doctors and other health care providers are guaranteed payment no matter how much they charge when a worker is injured on the job. The workers’ compensation system is broken.
The state, and the employers who pay into its workers’ compensation fund, have been paying two and three times the going rate for medical services when the patient is a workers’ compensation recipient. On average, surgeons charge 156 percent more, according to a report by the state’s Department of Insurance. Bills for radiology are 107 percent higher, 95 percent higher for occupational therapy and for something as simple as an ice pack, 300 percent more.
The extra paperwork required to document workers’ compensation cases and perhaps the added severity of the average injury, probably explains some of the price difference. But, human nature being what it is, it’s likely that, when the bill has to be paid no matter what the provider charges, the temptation to pad it can be irresistible, especially when providers can rationalize the surcharge by using it to offset underpayments in areas such as Medicare or Medicaid.
Lawmakers should make 2014 the last year that doctors and other health care providers are guaranteed payment no matter how much they charge when a worker is injured on the job. The workers’ compensation system is broken.
The state, and the employers who pay into its workers’ compensation fund, have been paying two and three times the going rate for medical services when the patient is a workers’ compensation recipient. On average, surgeons charge 156 percent more, according to a report by the state’s Department of Insurance. Bills for radiology are 107 percent higher, 95 percent higher for occupational therapy and for something as simple as an ice pack, 300 percent more.
The extra paperwork required to document workers’ compensation cases and perhaps the added severity of the average injury, probably explains some of the price difference. But, human nature being what it is, it’s likely that, when the bill has to be paid no matter what the provider charges, the temptation to pad it can be irresistible, especially when providers can rationalize the surcharge by using it to offset underpayments in areas such as Medicare or Medicaid.
Saturday, January 10, 2015
New Drugs to Treat Hearing Loss and Ear Disorders
A multitude of workers have occupational hearing losses induced by either sudden trauma or prolonged occupational exposures to loud noise. Some workers have hearing losses associated with age and fail to address the issue and create a potential safety concern in the workplace. In the past many have gone undetected and/or treated.
Workers' Compensation insurance provides for benefits for hearing losses and disorders associated with both traumatic (sudden) and occupational (exposure to loud noise) hearing losses occurring in the workplace. The insurance also allows workers to obtain hearing aids, treatment and medication(s).
Many of these conditions are not diagnosed or treated at an early stage for lack of attention. This is changing because of recent changes in medical delivery associated with the Affordable Care Act and Medicare. The new laws will afford millions a new opportunity to be diagnosed and treated.
Recent developments in pharmaceutical medicine may allow for restoration of hearing losses as well elimination of associated tinnitus, commonly known as ringing in the ears. Today's post is shared from nytimes.com/
Workers' Compensation insurance provides for benefits for hearing losses and disorders associated with both traumatic (sudden) and occupational (exposure to loud noise) hearing losses occurring in the workplace. The insurance also allows workers to obtain hearing aids, treatment and medication(s).
Many of these conditions are not diagnosed or treated at an early stage for lack of attention. This is changing because of recent changes in medical delivery associated with the Affordable Care Act and Medicare. The new laws will afford millions a new opportunity to be diagnosed and treated.
Recent developments in pharmaceutical medicine may allow for restoration of hearing losses as well elimination of associated tinnitus, commonly known as ringing in the ears. Today's post is shared from nytimes.com/
Wednesday, December 24, 2014
Where the Workers' Compensation Medical Dollar Goes in Florida
"Medical cost drivers, particularly in the areas of drugs, hospital inpatient, hospital
outpatient and ambulatory surgical centers (ASC) are noticeably higher in Florida than a
countrywide average. Legislative reform in the reimbursement of these services could
produce substantial savings for Florida employers. "
Florida Office of Insurance Regulation, Workers’ Compensation Annual Report December 2014
Related articles
- HHS Inspector General Scrutinizes Medicare Observation Care Policy (workers-compensation.blogspot.com)
- Fee Schedules and Value (workers-compensation.blogspot.com)
- Four Things You Should Know About Carpal Tunnel Syndrome (workers-compensation.blogspot.com)
- Wah, Wah, Wah (workers-compensation.blogspot.com)
- Medical Payments Per Claim in Florida Were Typical of Study States and Grew at a Moderate Rate From 2007 to 2012, Says New Study (workers-compensation.blogspot.com)
- Nebraska Supreme Court: Workers' comp includes PTSD, drug treatment after store shooting (workers-compensation.blogspot.com)
- Just Go to The Emergency Room (workers-compensation.blogspot.com)
- Using Workers' Compensation Records for Safety and Health Research (workers-compensation.blogspot.com)
- The Rule of Law and The Media's Role (workers-compensation.blogspot.com)
Tuesday, December 23, 2014
AbbVie Deal Heralds Changed Landscape for Hepatitis Drugs
Today's post is shared from NYTimes.com/ In a sign that price competition may take hold for hepatitis C drugs, the nation’s largest manager of prescriptions will require all patients to use AbbVie’s newly approved treatment rather than two widely used medicines from its rival Gilead Sciences. The pharmacy benefit manager, Express Scripts, said it had negotiated a significant discount from AbbVie in exchange for making the drugmaker’s treatment, Viekira Pak, the exclusive option for 25 million people. Express Scripts also said it would allow all people with hepatitis C to be treated with AbbVie’s drug, not only those with more serious liver damage. “We really believe we want all patients treated,” Dr. Steve Miller, the chief medical officer of Express Scripts, said in an interview Sunday. He said that AbbVie had made that affordable by offering “a significant discount.” Gilead’s drugs have set a new standard, curing the vast majority of patients in only 12 weeks with few side effects. But their prices have ignited an outcry. One drug, Sovaldi, has a list price of $84,000 for a typical 12-week course of therapy, or $1,000 per daily pill. The newer Harvoni costs $94,500 for 12 weeks. Gilead says the prices reflect the value the drugs bring to patients and the health care system. But some health plans, state Medicaid programs and prison systems say the drugs are busting their budgets. Many have been limiting treatment to only the sickest patients. Congress has... |
Related articles
- New Hepatitis C Drug Gets Helping Hand (wsj.com)
- Gilead Sciences sued over hepatitis C drug's $1000-a-pill price tag (mercurynews.com)
- Philadelphia Transportation Authority files lawsuit against Gilead over hepatitis C drug price (canadianbusiness.com)
Sunday, December 21, 2014
From the E.R. to the Courtroom: How Nonprofit Hospitals Are Seizing Patients’ Wages
This story was co-published with NPR and is shared from .propublica.org/ On the eastern edge of St. Joseph, Missouri, lies the small city's only hospital, a landmark of brick and glass. Music from a player piano greets visitors at the main entrance, and inside, the bright hallways seem endless. Long known as Heartland Regional Medical Center, the nonprofit hospital and its system of clinics recently rebranded. Now they're called Mosaic Life Care, because, their promotional materials say: "We offer much more than health care. We offer life care." Two miles away, at the rear of a low-slung building is a key piece of Mosaic—Heartland's very own for-profit debt collection agency. When patients receive care at Heartland and don't or can't pay, their bills often end up here at Northwest Financial Services. And if those patients don't meet Northwest's demands, their debts can make another, final stop: the Buchanan County Courthouse. From 2009 through 2013, Northwest filed more than 11,000 lawsuits. When it secured a judgment, as it typically did, Northwest was entitled to seize a hefty portion of a debtor's paycheck. During those years, the company garnished the pay of about 6,000... |
Related articles
- What We're Learning About Drug Company Payments to Doctors (workers-compensation.blogspot.com)
- Senior Care Workers Are Victims of Wage Violations (workers-compensation.blogspot.com)
- The Selling of Prescription Drugs: A Major Change in Sales Strategy (workers-compensation.blogspot.com)
- California Legislature Passes Bill to Protect Temp Workers (workers-compensation.blogspot.com)
- Senators Press Medicare for Answers on Drug Program (workers-compensation.blogspot.com)
- How Insurers Are Charging You More for Your Generic Drugs (workers-compensation.blogspot.com)
- Why Tylenol Isn't Always as Safe as People Think (workers-compensation.blogspot.com)
- Medicare's Failure to Track Doctors Wastes Billions on Name-Brand Drugs (workers-compensation.blogspot.com)
Subscribe to:
Posts (Atom)