The occupational healthcare program embodied in the recently enacted legislation has the potential for being the most extensive, effective and innovated system ever enacted for delivering medical care to injured workers. The “Libby Care” provisions, and its envisioned prodigies, will embrace more exposed workers, diseases and geographical locations, than any other program of the past. Potential pilot programs will now be available to injured workers and their families who have become victims of the failed workers’ compensation occupational disease medical care system.
The legislation initially establishes a program for the identification, monitoring and treatment of those who were exposed to asbestos in Libby Montana where W.R. Grace formerly operated an asbestos (vermiculite) mine producing, among other things, attic insulation. The plant belched thousands of pounds of asbestos fiber into the air of the geographical area daily. Libby Montana has been declared a Federal Superfund Site and the asbestos disease that remains as its legacy has been declared a National Public Health Emergency.
The newly enacted national health care law will have profound effect upon the treatment of occupational disease. Placed deep within the text of the bill (H.R. 3590), on page 836 (Section 1881A Medical Coverage for Individuals Exposed to Environmental Health Hazards), is the new occupational medical care model, “Libby Care.” The Manager’s Amendment, embracing the concept of universal occupational health care, inserted in the final moments of the debate, will make all the difference in world to the future of medical care and the handling of work-related illnesses.
What We Learned From History
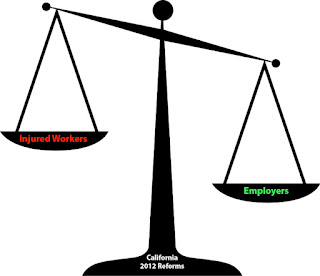
Historically it is well known that occupational diseases are problematic issues confronting workers’ compensation.They are problematic for all stakeholders in the system. For employers, it is difficult to defend a claim that may occur over a lengthy working period, ie. 280 days per year. Defending occupational disease claims has always been an elusive and a costly goal for employers and insurance carriers. Employees also are confronted with obstacles in obtaining timely medical benefits. Occupational disease claims are universally contested matter and medical care is therefore delayed until the claim is successfully litigated and potentially appealed. This process results in delay and denial of medical care and sometimes death.
In the 1950’s the insurance industry put tag-along verbiage in the statute to modify the 1911 workers’ compensation act to encompass occupational disease claims. This was not a philanthropic gesture, but one rather intended to shield Industry from rapidly spreading silicosis liability in civil actions emerging in the 1950s.
Over time, the failure of the workers’ compensation system to provide adequate medical care to injured workers suffering from occupational illness has given rise to the emergence of several attempted collateral benefit systems by the Federal government. The Black Lung Act-The Federal Coal Mine and Safety Act of 1969 established the Federal Black Lung Trust Fund, which obtained its revenue from the assessment of a percentage tonnage fee imposed on the entire Industry. In October 2000, the Federal government established The Energy Employees Occupational Compensation Program Act that provided a Federal bailout of liability for the monopolistic beryllium industry. The hastily enacted Smallpox Emergency Personnel Protection Act of 2003 (SEPA) shielded pharmaceutical manufacturers from liability. Following the horrific events of September 11, 2001, the Federal government quickly established The Victims Compensation Fund to compensate the victims and their families through an administrative system.
The largest transfer of economic wealth in the United States from Industry to the private sector, other than in the Attorney General’s thirty-eight State tobacco litigation, emanated from asbestos litigation which had its geneses in workers’ compensation. The late Irving Selikoff, MD’s pioneering efforts in providing expert testimony, based upon his sentinel studies of asbestos workers in Paterson, NJ, created the trigger mechanism for a massive wave of claims for occupational health care. The program never did adequately nor efficiently or expeditiously provide medical care.
The workers’ compensation system did not provide an adequate remedy because of a constellation of reasons, and subsequently, the wave spread to civil litigation out of desperation for adequate benefits. Asbestos litigation has been named, "The Longest Running Tort” in American history. While the Fairness in Asbestos Resolution Act of 2003, failed to be release from committee, the insurance industry tried to stifle the litigation but the effort failed. Asbestos litigation expanded into bankruptcy claims that continue unabated and the epidemic of disease continues. The remaining cases in the Federal court system were transferred to Federal Multi District Litigation (MDL 875) and the majority are finally concluding after twenty years of Panel consolidation. Medical benefits were not a direct component of that system. Unfortunately, asbestos is still not banned in the United States and the legacy of disease continues at historic rates.
The Costs
In a study prepared in 2000 by Dr. Steven Markowitz for a book entitled “Cost of Occupational Injuries and Illnesses”, it was revealed that the direct medical costs attributed to occupation illness by taxpayers, amount to $51.8 Billion dollars per year for the hospital physicians and pharmaceutical expenses. Overall workers’ compensation is covering 27% percent of the cost. This amounts to 3% of the National Gross National Product. The cost is passed on to: employers, insurance carriers, consumers, injured workers and the taxpayer. Medicare, a target of the cost shifting mechanism employer by Industry, continues its “pay and chase” policy in an effort to seek reimbursement under the Medicare Secondary Payer Act. All the stakeholders and the compensation systems have become increasingly bogged down as cost-shifting continues by Industry. The workers' compensation claims process has become stagnant.
Reportable Data A Questionable Affair
The quantification of occupational illness data has been very problematic as it is based on sources of questionable reliability. The US Bureau of Labor Statistics (BLS) based its collection on employer driven safety reporting, ieNCCI), keeps its data and procedures under wraps.
Both the NY Times and Nebraska Appleseed have reported that there exists underreporting of occupational disease conditions in epic proportions. They report that the elements of fear and intimidation directed to injured workers compound the defense attitude of employers and the insurance industry resulting in a massive underreporting of occupationally related medical conditions.
Increased Hurtles for Compensability
There have been attempts over the years to integrate more claims statutorily into the workers’ compensation system to shield employers from civil action and resultant large liability verdicts. This resulted in a flood of occupational exposure claims into the workers’ compensation arena. An effort in the mid-1980’s, following the asbestos litigation explosion, was by Industry to contain costs and restrict the payment of occupational disease claims even further in the workers’ compensation.
The initial effort was to create higher threshold standards and requirements in the area of mental stress claims. That was quickly followed by efforts to limit orthopedic and neurological carpal tunnel claims. Restrictive language interpreting what is peculiar to employment further limited all occupational disease claims.
Furthermore, scientific evidence proof requirements became increasingly difficult to surmount. Daubert type arguments emerged by the defense in the nations’ workers’ compensation forums where simplicity of a remedial and efficient benefit delivery program had existed in the past. Where a biological marker was not present, as was in asbestos exposure claims, the establishment of causal relationship was universally challenged.
Pre-existing and co-existing factors soon became other hurtles for injured workers and their families. Medical histories of orthopedic difficulties such as back conditions soon complicated repetitive motion trauma litigation. Co-existing and pre-existing smoking habits, family genetics and obesity were yet another obstacle to recovery.
Societal Habits Changed
Life and the way we look at work have changed dramatically with the onset of technology. Off-premises work is becoming more and more common with the advent of Internet access and economic globalization. Defining the barriers between work and pleasure has grown to be exceedingly difficult.
People are working harder and longer. More chronic conditions are prevalent in older workers. Disease increases with age and results in more total disability claims.
Occupational Medical Costs
The compensability of occupational claims is much more difficult to sustain in court. In recent studies over 99.9% of occupational deaths and 93.8% of the medical costs of occupational disease were held to be non-compensable. Over 50% of the lifetime medical costs are incurred during the last year of one’s life.
The Legacy of The Libby Montana Gold Rush
In 1881 gold miners discovered vermiculite, a form of asbestos in Libby, Montana. In 1920 The Zonolite Company was established and began to commercially mine vermiculite. W.R. Grace bought the mining operations in 1963. In 1990 the mine was closed and production ended.
For decades W.R. Grace belched over 5,000 pounds of asbestos into the air in and around Libby on a daily basis. The residents who worked at the plant and their families and household contacts were exposed to asbestos fiber. Mineworkers brought home the asbestos on their clothing. The unknowing inhabitants and their families used the asbestos to fill their gardens, their driveways, the high school track, the little league field and in their attics for insulation.
The US Environmental Protection Agency (EPA) visited Libby in 1999 and investigated the incidence of disease and the contamination of the site. The EPA declared Libby a Superfund site in October 2002 and a physical clean-up began of the geographical area. The question of who would pay for the medical care of Libby remained an unknown.
A Manager’s Amendment
Senator Max Baucus (D-MT), Chair of the Senate Finance Committee, utilizing a mechanism known as “A Manager’s Amendment,” at the last moment, modified the Senate’s version of the Health Care Reform Bill. The Patient Protection and Affordable Care Act passed the Senate, ultimate cleared the House and was signed into law by President Obama on March 23, 2010. Section 10323, Medicare Coverage for Individuals Exposed to Environmental Health Hazards, 2009 Cong US HR 3590, 111th Congress, 1st Session (December 31, 2009).
Senator Bacus said, “This provision is important because it will provide vital medical services to American who—through no fault of their own—have suffered horrible effects from their exposure to deadly poisons. It will provide vital medical services we owe these Americans under our commitment in the Superfund Act.” The amendment initially provides for screening and medical care to residents of the Libby Montana asbestos contaminated site that was owned and operated by W.R. Grace. It essentially provides for universal health care.
“Libby Care” Is The New Occupational Medical Care Model Legislation
The Libby site qualified for the medical program because the hazardous asbestos contaminated site in Libby was deemed to be “a public health emergency” on June 17, 2009 as defined by the Comprehensive Environmental Response, Compensation, and Liability Act of 1980 (CERCLA). While there are 1700 designated Superfund sites, Libby is the first site in the history of the program that has been designated as “a public health emergency.” The program may be expanded in adopted to other communities at the discretion of the Secretary of of the Department of Health and Human Services (HHS).
The plan authorizes a grant for initial medical screening purposes. The screening would determine if a medical condition is present that is attributable to the environmental exposure. It allows those individuals with a diagnosed medical condition due to the environmental exposure at the site to get Medicare services. The Secretary of the Department of HHS may establish additional pilot programs to provide additional medical care appropriate for the residents of contaminated communities so designated. The delivery of Medicare medical benefits will be directed to those “who have suffered horrible effects from their exposure to deadly poisons.”
The purpose of the legislation is “…. to furnish such comprehensive, coordinated and cost-effective care to individuals…..” p2224 l3-1. It mandates the furnishing of “Flexible Benefits and Services,” for items, benefits or services NOT covered or authorized by the Act. It further authorizes the institution of “Innovative Reimbursement Methodologies,” for reimbursement subject to offsets for individuals “eligible to receive public or private plan benefits or legal agreement.” p2226 ll8-11. The Secretary of HHS will maintain “waiver authority.”
Charting A New Course
After a century of struggle, the United States now embarks upon a new course for occupational medical care. The law charts a new path for the delivery of occupational disease medical benefits on a timely basis. It will permit researchers an avenue for the collection of epidemiological data so that the workplace can be made safer. All will benefit. The innovative legislation provides for a long awaited and much needed initiative to provide an efficient, responsive and coordinated treatment plan and preventive health program that hopefully will expand and will vastly improve occupational health care.